Module One: Our Journey
This module provides an introduction and welcome to Yorta Yorta country and includes historical context from a global, national and local perspective.
Aboriginal Cultural Competency is a continuum and we are all at some point along that continuum depending on the level of professional experience, knowledge, values, beliefs and life experience we may have in our lives. Even Aboriginal people are at different points along that continuum depending on their opportunities for living and learning in their Aboriginal communities and families.
This module provides an introduction and welcome to Yorta Yorta country and includes historical context from a global, national and local perspective.

This module provides a broad snapshot of our Aboriginal way of life and experiences, and then localises that view for your time here working and

This Module discusses approaches to Aboriginal health and wellbeing from the context of the Aboriginal and non-Aboriginal service sector specifically. This is critical for your

VIDEO CASE STUDIES Module Overview Throughout this Cultural Competency package, we have talked about a range of factors relating to Aboriginal health and wellbeing, and
Disclaimer: Respecting Aboriginal People, Culture and Communities:
This resource has been developed by Robynne Nelson of Healing the Spirit Pty Ltd (Trading as Mulana Kaalinya) for use by Melbourne University UDRH across Yorta Yorta Country and Ballarat UDRH specifically.
This curriculum is focussed primarily on the Aboriginal cultural competency learning needs of Melbourne University UDRH students whilst studying or undertaking placement on Yorta Yorta country. Whilst the resource provides a national historical context it by no way attempts to cross over into the cultural values, beliefs and practices of Aboriginal people living off Yorta Yorta country.
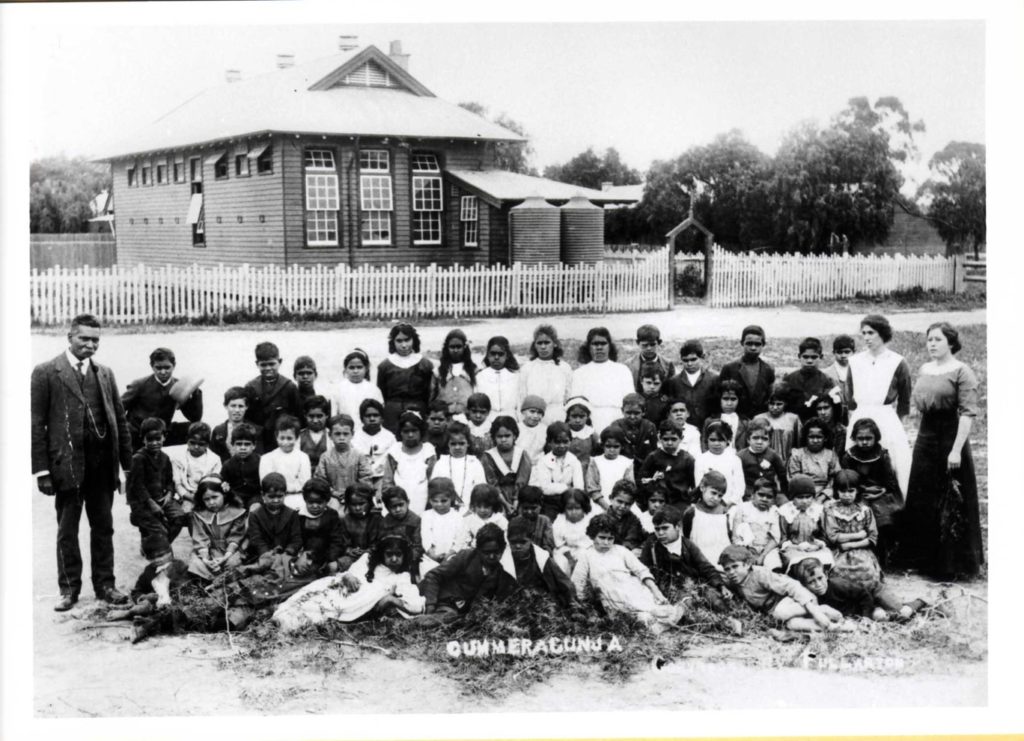
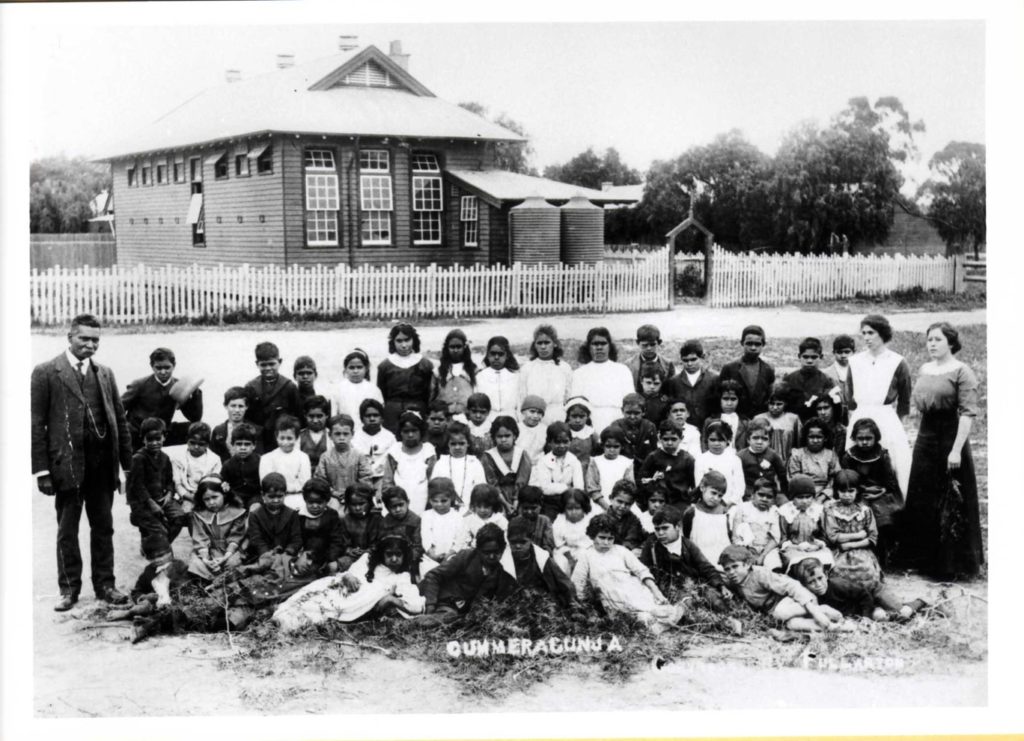
Videos and photos are included in this resource and may contain images or audio of people who have since deceased. No specific men’s or women’s business, family business, or taboo topics have been discussed within this resource.

DEPARTMENT OF RURAL HEALTH
Going Rural Health is an initiative to support health student’s complete rural clinical placements. This programme is gratefully funded by the Australian Government Department of Health and is open to students from all nationally recognised tertiary education providers.
Copyright © This resource has been developed by Robynne Nelson of Healing the Spirit Pty Ltd for use by Melbourne University UDRH across Yorta Yorta Country, Wodonga, and Ballarat UDRH specifically.
Throughout Module Two we had talked about Culture, Cultural Identity, How Culture Impacts Health, and Cultural Safety, all of which clearly highlight the importance of identifying Aboriginal people, so that you as professionals and clinicians can support Aboriginal people appropriately and act in a more culturally sensitive and specific way.
This definition is a three-part definition requiring all 3 parts to be established for Aboriginality to be recognised:
Reference: www.naccho.org.au
Most Aboriginal people are not asked to ‘prove’ Aboriginality today, but to ‘confirm’ which has a much nicer connotation to it. Asking people to prove it is a quite forceful way to approach that question, particularly as so many are already feeling disenfranchised e.g., stolen generation members.
Closing the Health Gap framework requires the Aboriginality question to be asked of every patient entering your service. This question is also asked across most sectors of the community today e.g. education, justice, employment, housing, aged care and disability, and child and family services etc. The identification of Aboriginal people then provides services with the capacity to provide support, and guides services as to the types of services and approaches to service delivery that may be needed.
Identifying Aboriginality opens the dialogue between physicians and Aboriginal patients as to their cultural and spiritual needs whilst at that service, in that hospital, or receiving palliative care. If an Aboriginal Elder is in the final stages of life, it opens the conversations as to the Elders spiritual needs e.g. Would they like to be visited by their Church Pastor, or do they want an Aboriginal Elder to visit and complete a smoking ceremony or other rituals to help them on their final journey to the Dreaming?
For example, across the health sector and with Closing the Health Gap in place, this question will have multiple impacts on your work with Aboriginal patients including:
This question has been known to be asked in a wide range of appropriate and inappropriate ways – and at times staff e.g. admissions at hospitals, may avoid asking the question out of fear of embarrassing someone by asking it. That attitude itself may be offensive. This question should be asked just like any other question such as religion, date of birth, medical issues and so forth. It is then up to the patient/individual to answer as they feel comfortable.
This question is asked in two different ways across services:
Question One: “Are you of Aboriginal or Torres Strait Islander descent?” OR
Question Two: “Do you identify as Aboriginal or Torres Strait Islander?”
Both can generate very different responses.
So, which is the right way? As a consultant and nurse of over twenty years, I have my own personal view about these questions, and want to throw a spanner in the works.
If you ask:
If you ask:
Going back to the first question about descent – if they are more likely to say “yes, but I don’t want you to put it down”, you at-least know that they are. You can honour their request not to document their Aboriginality. However, you can then also still consider some aspects of their care and your approach regardless. This means you may still act in a culturally sensitive way, consider health factors of concern for Aboriginal people as part of a health assessment, and you may still need to be mindful of extended family, communication, health literacy, and cultural needs.
Of course, you will be required to abide by your employers policies and procedures, and the appropriate question as outlined on their documentation, but now you can also be more mindful and be open for debate amongst you peers about this question. What is most paramount, is that the patient/client receives the most appropriate care for their needs, to gain the best outcome.
E.g. you may have known them all your life, went to school together and never knew them as Aboriginal.
Aboriginality is not for you as a professional person to challenge. You can only take the word of a client/patient. It is expected that Aboriginal community organisations will address such matters in due course when a Confirmation of Aboriginality is required, or an Aboriginal staff member is in the position to question and ask for confirmation.
Identifying Aboriginal people is reliant on the willingness of services to ask about Aboriginality, document clearly, understand why they are asking and being able to explain to others how that information is used. It’s also reliant on Aboriginal people feeling safe enough to respond honestly without fear.
If you don’t understand the definition of Aboriginality and make your own judgments, don’t understand why the question is asked, fail to ask, or ask in an inappropriate way, a range of negative outcomes can follow.
